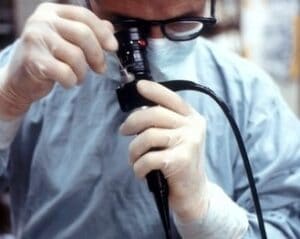
 Hospitals are beginning to spend a lot of time planning for a post-Covid environment. However, one lasting effect of Covid-19 will be the constant focus on infectious diseases and preventing the next pandemic from occurring. Endoscopes, as instruments that have been linked with many superbug outbreaks in the recent past, need another look to make sure that proper cleaning protocols are in place at every hospital.
Hospitals are beginning to spend a lot of time planning for a post-Covid environment. However, one lasting effect of Covid-19 will be the constant focus on infectious diseases and preventing the next pandemic from occurring. Endoscopes, as instruments that have been linked with many superbug outbreaks in the recent past, need another look to make sure that proper cleaning protocols are in place at every hospital.
Linda Spaulding, a prominent infection control specialist, recently outlined her concerns about endoscope reprocessing, and what hospitals can look to improve in the process. This article by Frank Diamond at Infection Control Today explains Ms. Spaulding’s concerns:
“You can be told you’re going to be the endoscopy scope cleaner, or tech. They’ll bring you in, they will work with you, show you. Put you through training on how to clean the scope. Show you where everything is. And then you’re the endoscopy cleaning person. In some hospitals, it might be a nurse, because the nurse is helping the physician do the scope, then the nurse is cleaning the scope afterwards, getting it ready to use on the next patient and the next doctor who is coming in. You could see how shortcuts could be taken. And so, anybody can be trained to clean the scope. It’s just how well are they trained? And is the person training them really doing it correctly? And usually when we have outbreaks in these areas, we find that somebody was trained wrong. Or somebody says, “Yes, I follow all the steps that’s on this poster.” And then when you observe them, you find out they missed one or two steps. Those one or two steps are critical. We were talking about central line infections in another talk. I think I brought it up. It’s the same thing. If somebody’s not visually verifying and validating that the person is still doing it right, even if that person has been there 25 years, then things can go wrong, and you can end up with infections. You have some people that have been there 25 years. All they’ve done is scope cleaning. “Of course, I’m really good at it. I’ve been doing it for 25 years.” Yet we still find shortcuts. Because somewhere in their career, they decided to take a shortcut because they had to turn the scope over really fast. And then it’s like, “Oh, well, it worked that time. I’ll just keep doing it this way, because it’s quicker.” And nobody’s going to know that there’s an outbreak from endoscopes until enough physicians identify for themselves that, “Oh, I have a patient that got infected.” Then they hear from another doc. “You know, I have a patient that got infected after an endoscope.” And then they hear the third doc. And then the docs kind of put it together. “Wait a minute, there are three patients that had endoscopes here.” But if each physician is only seeing one at a time, nobody’s putting it all together that there’s a problem because the likelihood of one physician—unless he’s the only one that does the endoscopes—being able to identify an infection and [know how many people got infected is unlikely.] And if the docs aren’t talking and sharing that information, then nobody really knows until you have a whole lot of people infected.”
Read the entire article here: Endoscope Cleaning: What Infection Preventionists Should Know
As Ms. Spaulding points out, the infection risk with high-level disinfected endoscopes will continue to be a major source of concern for hospitals. Facilities must ensure staff are trained on general infection control principles and reprocessing best practices, and they must be prepared to constantly monitor and improve their practices. To ensure that your staff is following reprocessing best practices on every scope they disinfect or sterilize, install additional checks and balances into your workflow so that you can document that your staff is following the same process each time. Endoscope tracking systems such as iRIScope have been introduced in recent years to help hospitals and surgery centers ensure that each of their flexible endoscopes is reprocessed the proper way each time, and documentation of their reprocessing is kept electronically using advanced RFID technology. These systems safeguard the scope disinfection process by employing artificial intelligence to determine if scopes are adequately reprocessed before their next use. With these systems in place, staff can be more confident that their endoscope-related procedure won’t result in a superbug outbreak.
